difference between rough endoplasmic reticulum and smooth endoplasmic reticulum
Anatomy books
Thursday, December 28, 2023
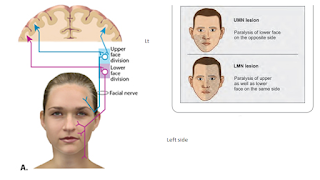
Bell palsy vs facial palsy due to stroke
Bell palsy vs facial palsy due to stroke
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
The two most common causes of acute facial paralysis are Bell’s palsy and ischemic stroke or upper motor type of facial paralysis.
Facial weakness can be caused by strokes in many different locations in the brain and brainstem. Strokes involving the brain typically cause central facial weakness that involves the mouth and spares the eye and forehead.
Strokes involving the brainstem can sometimes cause weakness of the mouth, eye and forehead–mimicking a peripheral lesion. In these cases however, there will be other focal neurologic deficits. A review of systems and neurologic examination can help to identify signs and symptoms of stroke.
Bell's palsy is a condition that causes sudden weakness in the muscles on one side of the face. In most cases, the weakness is temporary and significantly improves over weeks.
The weakness makes half of the face appear to droop. Smiles are one-sided, and the eye on the affected side resists closing.
Bell palsy vs facial palsy due to stroke
Topic | Upper motor type/ stroke | Lower motor type/ bell’s palsy | |
Age | >60 years | 20 -50 | |
Time course | Second to minutes | Few hours to few days | |
Upper face | Usually not affected | Affected | |
Lower face | Affected | Affected | |
Associate symptoms | • Rapid onset of mild weakness to total paralysis on one side of your face — occurring within hours to days • Facial droop and difficulty making facial expressions, such as closing your eye or smiling • Drooling • Pain around the jaw or in or behind your ear on the affected side • Increased sensitivity to sound on the affected side • Headache • A loss of taste • Changes in the amount of tears and saliva you produce | stroke causing isolated left lower facial weakness. There’s a flattened nasolabial fold & inability to smile on the affected side with sparing of the forehead & eye closure muscles. Weakness or numbness in the arm or leg: Weakness or numbness can occur either on the same side as the facial palsy, or on the opposite side, Difficulty swallowing (dysphagia): Dysphagia secondary to brainstem ischemia | |
 |
Difference between corticospinal tract and corticonuclear tract
Difference between corticospinal tract and corticonuclear tract
<script async src="https://pagead2.googlesyndication.com/pagead/js/adsbygoogle.js?client=ca-pub-1234567890123456" crossorigin="anonymous"></script>
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
Corticonuclear tract | Corticospinal tract |
Definition: motor pathway from the motor cortex of the brain to the motor nuclei of cranial nerves within the brainstem. | Definition: motor pathway from the brain’s motor cortex to lower motor neurons located in the anterior horn of the spinal cord’s gray matter. Divided into the anterior corticospinal tract (supplies axial muscles) and the lateral corticospinal tract (supplies muscles of the limbs). |
Function: responsible for voluntary movement of the muscles of the face (CN. VII), head and neck (CN. XI). Also involved in phonation, swallowing and facial expression. (CN. VII and IX) | Function: responsible for voluntary movement of the muscles of the limbs and trunk. |
Difference between connective tissue mast cell and mucosal mast cell
Difference between connective tissue mast cell and mucosal mast cell
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
Topics | connective tissue mast cell | mucosal mast cell |
Another name | Also known as MCTC mast cell | Also known as MCT mast cell |
Location | Skin , intestinal submucosa, breast and axillary lymph nodes | Lungs, intestinal mucosa |
Granules and its internal structure | Granules with Lattice like internal structure | Granule with a scroll like internal structure |
Granules contain | Tryptase and chymase | Only tryptase |
Differences between the electrical and chemical synapses.
Differences between the electrical and chemical synapses.
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
Chemical synapses | Electrical synapses |
It is present in higher vertebrates. | It is present in both lower and higher vertebrates and invertebrates. |
Nerve impulse is transmitted using a neurotransmitter. | Nerve impulse is transmitted using ions. |
Unidirectional transmission. | Bi-directional transmission. |
Gaps between cells are around 20 nm | Smaller gaps - only 3 - 5 nm |
Transmission is relatively slow - several milliseconds. | Transmission is fast - almost instant. |
Either inhibitory or excitatory. | Excitatory. |
Signal remains strong. | Signal will disappear over time. |
Sensitive to pH and hypoxia. | Insensitive to pH and hypoxia. |
Vulnerability to fatigue. | Relatively less vulnerable to fatigue. |
Difference between pulsation of jugular vein and carotid artery
Difference between pulsation of jugular vein and carotid artery
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
PULSATION OF JUGULAR VEIN | PULSATION OF CAROTID ARTERY |
No pulsations palpable. | Palpable pulsations. |
Pulsations obliterated by pressure above the clavicle. | Pulsations not obliterated by pressure above the clavicle. |
Level of pulse wave decreased on inspiration; increased on expiration. | No effects of respiration on pulse. |
Usually two pulsations per systole (x and y descents). | One pulsation per systole. |
Prominent descents. | Descents not prominent. |
Pulsations sometimes more prominent with abdominal pressure. | No effect of abdominal pressure on pulsation |
Thursday, February 23, 2023
Anatomy of thyroid cartilage
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
My blog: Difference between : http://www.microscopicanatomybd.blogspot.com
The thyroid cartilage is a substantial shield-shaped structure that is situated near the top of the larynx in the front of the neck (voice box). Due to variations in the size and shape of the larynx, it is frequently referred to as the Adam's apple and is more noticeable in men than in women.
The laryngeal prominence, also referred to as the Adam's apple, is the point where the two halves or plates of hyaline cartilage that make up the thyroid cartilage meet. The superior thyroid notch, which is modest and visible in certain persons, is located in front of the thyroid cartilage.
The larynx and vocal cords are shielded by the thyroid cartilage, which is also crucial for speech production. The muscles of the larynx are in charge of regulating the tension and positioning of the vocal cords during speech and singing. The vocal cords are linked to the rear of the thyroid cartilage. By providing places of attachment for the muscles involved in swallowing, the thyroid cartilage also contributes to this process.
Skin superficial fascia and deep fascia of neck Gold information to memorize
Skin superficial fascia and deep fascia of neck Gold information to memorize
For learning anatomy, please visit :
My youtube channel : @easyhumanatomy73
My website : http://easyhumananatomy.com
My facebook page: https://www.facebook.com/easyhumanatomy/
My blog: http://www.easyhumanatomy73.blogspot.com
|
1.
All cutaneous nerve of
neck are derived from cervical plexus except |
greater occipital nerve
which is derived from dorsal ramus of C2 spinal nerve |
|
Thickest cutaneous nerve of the body |
Greater occipital nerve |
|
Cutaneous nerve which may pierce clavicle through
and through |
Intermediate supraclavicular nerve |
|
Most important superficial vein in the neck |
external jugular vein |
|
Most commonly used external jugular vein for
central venous cannulation catheterization |
right external jugular
vein |
|
Muscle of neck representing panniculus carnosus of
lower animals |
Platysma |
|
Cold abscess (tubercular abscess) abscess without
signs of acute inflammation like pain and redness Commonest cause of cold abscess in the neck |
Tuberculosis of cervical vertebrae |
|
Fibrous band connecting thyroid capsule to the
cricoid cartilage |
Ligament of Berry |
Submandibular region, Gold information to memorize
Submandibular region
Gold information to memorize
1.
Key muscle of submandibular
region
Ans: Hyoglossus
2.
Smallest of the three parts
of large salivary glands
Ans : Sublingual
salivary gland
3.
Wharton duct
Ans: Submandibular
duct
4.
Ducts of Rivinus
Ans: Ducts
of sublingual gland
5.
Langley ganglion
Ans: Submandibular
ganglion
6.
Most commonly damaged artery
during surgical removal of submandibular gland
Ans facial artery
7.
Most commonly damaged nerve
during surgical removal of submandibular gland
Ans : lingual nerve damaged
during ligation and divison of submandibular duct
Clinical anatomy of scalp
Clinical anatomy of
scalp
1. Which layers of scalp is known as dangerous
layer of scalp?
·
4th layer, the subaponeurotic
layer of scalp is known as dangerous layer of scalp.
·
Why
?
·
Due to loose spaces blood and pus tent to
collect in this space and this space contain emissary veins which connect veins
of scalp to the venous sinuses of cranium. So infection from this layer spread
into the venous sinuses of cranium.
2. Functional importance of sub aponeurotic
layer of scalp
·
In case children injury of vault, blood from
intra cranial hematoma accumulate in 4th layer of scalp, so no sign
of intracranial pressure rise was seen
3. Why bleeding
under surface of periosteum of skull bone cause cephalohaematoma
It is a hemorrhage of blood between the skull and the
periosteum of particular skull bones. It is a typically harmless condition that causes
blood to pool under a newborn's scalp after a difficult vaginal delivery.
Periosteum of skull bone, the innermost layer of scalp is loosely attach to
bone except near the suture, so hemorrhage below this layer make shape of
individual bone. It is more see in parietal region.
4. Why a blow on head
lead to “black eye’ ?
·
Injury of the scalp causes collection of
blood into the 4th layer of scalp, the sub-aponeurotic layer of
scalp. Frontalis muscle which cover part of forehead of scalp has no bony
attachment and due to gravity blood accumulated in the scalp go downward and
accumulate under the eye.
5. After scalp injury,
why blood accumulate under the eye but not goes laterally and posteriorly.?
·
The epicranial aponeurosis of scalp and
occipitalis muscles have bony attachments to superficial temporal lines and
superior nuchal lines, so blood cannot go laterally and posteriorly but frontalis muscle has no bony attachment
so blood always track downward and settle under the eye.
6. Why wounds of scalp
bleed profusely?
·
It has two causes
·
The scalp is rich in blood supply
·
For epicranial aponeurosis (or galea
aponeurotica) which is a tough layer form by dense fibrous tissue and scalp blood vessel adhere with it which
prevent vasocontriction , so scalp injury bleed more.
7. Why transverse scalp injury tend to create more gap?
Ans Epicranial
aponeurosis (or galea aponeurotica), the 2nd layers of the scalp
which is a tough layer made by dense fibrous tissue which runs from the
frontalis muscle anteriorly to the occipitalis posteriorly. So there is a tension present within the epicranial
aponeurosis from anterior posteriorly. So a large gap is created when injury
occur in transversely but injury occur in anterior posterior direction is not
followed by large gap.
8.
Caput succedaneum is swelling of the scalp in a newborn. It is most often brought on by pressure from the
uterus or vaginal wall during a head-first (vertex) delivery.
9.
Clinical anatomy of Caput succedaneum
It is swelling due to collection of fluid in the 4th layer(loose areolar tissue) of scalp in a newborn. It is most often brought on by pressure from the uterus or
vaginal wall during a head-first (vertex) delivery. It is subsides
with 1-2 days



